Avoid Costly HIPAA Fines: How a Solid Business Associate Agreement Protects Your Practice
Healthcare businesses face an increasingly complex regulatory landscape where a single compliance mistake can result in devastating financial...
9 min read
LegalGPS : Dec. 12, 2025
Telemedicine revolutionized healthcare delivery, especially during the pandemic when virtual visits became essential. However, this digital transformation created a complex web of legal risks that many healthcare providers never anticipated. What seemed like a simple transition to video calls has exposed practices to licensing violations, malpractice claims, and regulatory penalties that can devastate a medical practice.

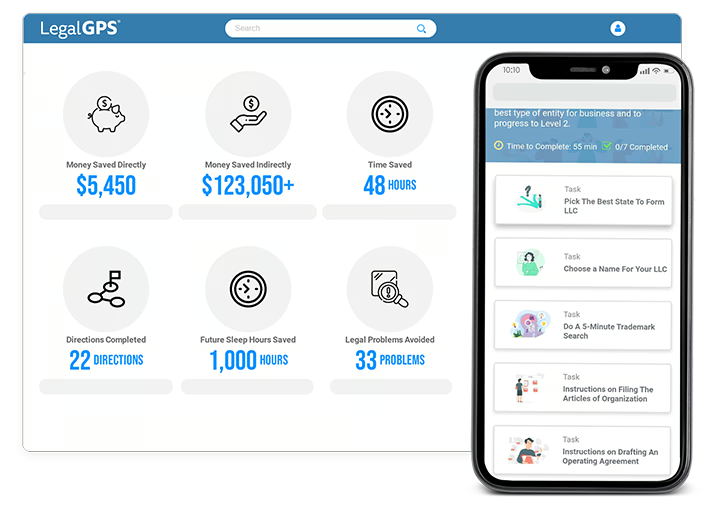
Legal GPS Pro
Protect your business with our complete legal subscription service, designed by top startup attorneys.
The legal landscape for telemedicine differs dramatically from traditional in-person care. State licensing boards, federal agencies, and insurance companies each impose distinct requirements that vary significantly across jurisdictions. Many providers discover these obligations only after facing penalties or legal action.
Understanding these risks isn't just about compliance—it's about protecting your practice, your patients, and your professional reputation. The consequences of telemedicine legal missteps can include state board sanctions, federal investigations, malpractice lawsuits, and financial penalties that reach hundreds of thousands of dollars.
Telemedicine Service Agreement for virtual healthcare delivery, privacy, and compliance.
Trusted by 1,000+ businesses to safeguard their LLCs.
Telemedicine practice requires careful attention to state licensing requirements that many providers overlook. Each state maintains its own medical licensing authority, and providing care to patients in different states often requires additional licenses or special permissions. The interstate nature of telemedicine creates jurisdictional complexities that don't exist in traditional practice.
Most states require physicians to hold an active license in the state where the patient is located during the telemedicine encounter. This means treating a patient vacationing in Florida while you're licensed only in New York could constitute unlicensed practice of medicine. Some states offer telemedicine-specific licenses or participate in interstate compacts, but coverage remains inconsistent.
Dr. Elena Martinez, an internal medicine physician in Texas, began offering telemedicine consultations to expand her practice reach. She regularly treated patients across several neighboring states without researching licensing requirements. When a patient in Louisiana filed a complaint about their treatment, the Louisiana State Board of Medical Examiners launched an investigation.
The board discovered Dr. Martinez had been practicing medicine in Louisiana without a license for over eighteen months. They imposed a $45,000 fine and required her to cease all Louisiana patient care immediately. The incident also triggered a review by her Texas medical board, resulting in additional professional monitoring requirements. Dr. Martinez spent over $30,000 in legal fees resolving the matter and lost substantial revenue from discontinued patient relationships.
The interstate medical licensing compact provides some relief, but only participating states recognize compact licenses. Even within compact states, certain practice restrictions may apply. Providers must verify their licensing status for each state where they intend to treat patients via telemedicine.
Hospital credentialing presents additional challenges for telemedicine providers. Many health systems require separate credentialing processes for telemedicine services, even for physicians already credentialed for in-person care. These requirements can significantly delay telemedicine program implementation.
Healthcare privacy regulations become significantly more complex in telemedicine environments. HIPAA requirements apply to all patient interactions, but virtual care introduces new risks around data transmission, storage, and third-party access. The technology platforms used for telemedicine must meet specific security standards that many consumer-grade video conferencing solutions cannot provide.
Protected health information transmitted during telemedicine encounters requires end-to-end encryption and secure storage protocols. Providers must ensure their chosen platforms include business associate agreements that properly allocate HIPAA liability. Many popular video conferencing tools explicitly exclude healthcare use from their terms of service, creating potential compliance gaps.
Patient privacy extends beyond the technology platform to include the physical environments where telemedicine occurs. Providers must control their surroundings to prevent unauthorized individuals from overhearing patient conversations. Similarly, patients may be in shared living spaces or public locations that compromise confidentiality.
Before implementing any telemedicine program, verify that your technology platform includes encryption for data in transit and at rest, signed business associate agreements with all technology vendors, user authentication and access controls, automatic session timeouts for idle connections, and audit logging capabilities for all platform access. Establish protocols for verifying patient identity at the start of each session, confirming the patient's location and privacy level, documenting any privacy limitations or interruptions, and securing any recorded sessions according to your retention policies.
Train all staff on telemedicine-specific privacy requirements and create incident response procedures for potential breaches occurring during virtual care. Regular privacy risk assessments should include evaluation of new telemedicine technologies and evolving regulatory requirements.
Informed consent requirements for telemedicine differ substantially from in-person care protocols. Providers must clearly explain the limitations of virtual examinations, technology risks, and emergency procedures when patients aren't physically present. Standard consent forms designed for office visits often fail to address telemedicine-specific considerations.
Patients must understand what clinical information can and cannot be obtained through virtual examination. The limitations of remote physical assessment, inability to perform certain diagnostic procedures, and potential delays in emergency response require specific disclosure. Documentation must reflect these discussions and patient acknowledgment of telemedicine limitations.
The Thompson family sued pediatrician Dr. James Wilson after their eight-year-old son experienced complications following a telemedicine consultation. During the virtual visit, Dr. Wilson diagnosed a minor respiratory infection and prescribed antibiotics without conducting a physical examination. The child's condition worsened overnight, requiring emergency hospitalization for pneumonia.
The family's legal team argued that proper informed consent would have included discussion of physical examination limitations and recommendations for in-person evaluation when symptoms persisted. Dr. Wilson's documentation showed no evidence of informed consent discussions specific to telemedicine limitations. His standard office consent forms didn't address virtual care restrictions or emergency protocols.
The case settled for $125,000, with Dr. Wilson's malpractice carrier requiring implementation of comprehensive telemedicine consent procedures. The settlement included requirements for documented informed consent discussions, clear emergency contact protocols, and specific documentation of telemedicine examination limitations. Dr. Wilson also faced medical board review of his telemedicine practices and additional continuing education requirements.
Emergency response protocols represent a critical component of telemedicine informed consent. Patients must understand how to access emergency care when their provider isn't immediately available. Clear documentation of patient location and local emergency contact information becomes essential for virtual care providers.
State regulations increasingly require specific informed consent elements for telemedicine encounters. These may include disclosure of provider licensing information, explanation of technology platform security measures, and confirmation of patient identity verification procedures.
Medical malpractice liability in telemedicine encompasses unique considerations that don't exist in traditional practice settings. The standard of care for virtual encounters may differ from in-person consultations, but courts haven't established consistent guidelines for these differences. Providers face uncertainty about how their telemedicine decisions will be evaluated in potential malpractice cases.
Diagnostic limitations inherent in virtual examinations create specific liability risks that providers must carefully manage. The inability to perform hands-on physical examinations, conduct certain diagnostic tests, or observe subtle clinical signs may impact diagnostic accuracy. Documentation must clearly reflect these limitations and the clinical reasoning behind diagnostic and treatment decisions.
Dr. Sarah Chen conducted a telemedicine consultation with Michael Rodriguez, who complained of severe abdominal pain. During the 15-minute virtual visit, Mr. Rodriguez appeared uncomfortable but was able to communicate clearly. Dr. Chen recommended over-the-counter pain medication and scheduled a follow-up appointment for the following week, noting that the patient didn't appear to be in acute distress.
Six hours later, Mr. Rodriguez was rushed to the emergency room with a ruptured appendix requiring immediate surgery. His condition had deteriorated rapidly after the telemedicine consultation. The emergency physician noted that certain clinical signs of appendicitis might have been detectable during an in-person examination but weren't apparent during the virtual visit.
Mr. Rodriguez filed a malpractice lawsuit claiming Dr. Chen failed to meet the appropriate standard of care by not recommending immediate in-person evaluation or emergency room consultation. Expert witnesses disagreed about whether the telemedicine examination provided sufficient information for proper diagnosis. The case highlighted the challenge of establishing standard of care protocols for virtual consultations when serious conditions may not be immediately apparent through video examination.
The lawsuit ultimately settled confidentially, but Dr. Chen faced significant legal expenses and reputation damage. Her malpractice insurance premiums increased substantially, and she implemented new protocols requiring in-person evaluation for certain symptom presentations that might indicate serious underlying conditions.
Clinical decision-making in telemedicine requires heightened attention to documentation that supports the appropriateness of virtual care for specific patient presentations. Providers must clearly articulate why telemedicine was suitable for each encounter and what alternative recommendations were considered.
Maintain detailed documentation explaining why telemedicine was appropriate for each specific patient encounter and symptom presentation. Record all clinical observations possible through virtual examination, including patient appearance, speech patterns, mobility, and environmental factors. Document any limitations of the virtual examination and how these limitations influenced your clinical decision-making.
Include specific rationale for prescribing or not prescribing medications based on virtual assessment capabilities. Note any recommendations for in-person follow-up, emergency evaluation, or additional diagnostic testing. Document patient compliance with safety instructions and their understanding of when to seek emergency care.
Create standardized documentation templates that prompt inclusion of telemedicine-specific clinical reasoning. Regular chart review should ensure documentation adequately supports the clinical decisions made during virtual encounters.
The technology infrastructure supporting telemedicine creates distinct legal obligations that extend beyond basic HIPAA compliance. Platform selection, vendor contracts, and system reliability directly impact provider liability and regulatory compliance. Many healthcare providers underestimate the legal significance of their technology choices until problems arise.
Business associate agreements with technology vendors must clearly allocate responsibility for security breaches, system downtime, and regulatory compliance. Standard vendor contracts often contain liability limitations that leave healthcare providers exposed to significant financial risk. Negotiating appropriate vendor accountability requires careful attention to contract terms that many providers overlook.
Regional Healthcare Network relied on TeleMed Solutions for their comprehensive telemedicine program serving rural communities. The platform handled hundreds of patient encounters daily, including urgent care consultations and chronic disease management. When a major system failure occurred during a winter storm, patients lost access to critical medical services for over 48 hours.
During the outage, patient Margaret Foster attempted to reach her cardiologist for medication adjustment guidance. Unable to connect through the telemedicine platform, she increased her medication dosage based on previous instructions. This decision led to dangerous drug interactions and emergency hospitalization. Mrs. Foster suffered permanent kidney damage requiring ongoing dialysis treatment.
The resulting lawsuit revealed that TeleMed Solutions' contract limited their liability to the monthly service fee, approximately $500. Regional Healthcare Network faced the full burden of damages, ultimately settling for $2.3 million. The incident exposed inadequate backup communication systems and insufficient patient notification procedures during platform failures.
Investigation showed that Regional Healthcare Network had failed to verify TeleMed Solutions' business insurance coverage or establish alternative communication protocols for system outages. Their contract didn't require minimum uptime guarantees or specify emergency response procedures when technology failures occurred.
System reliability requirements should include specific uptime guarantees, redundant communication methods, and clear escalation procedures for technical failures. Providers must maintain alternative communication channels for urgent patient needs when primary telemedicine platforms experience problems.
Data ownership and portability clauses in vendor contracts become critical if providers need to change technology platforms. Patient records, communication histories, and clinical data must remain accessible regardless of vendor relationship changes.
Prescribing medications through telemedicine encounters involves complex federal and state regulations that vary significantly by drug classification and patient relationship. The Drug Enforcement Administration maintains specific requirements for prescribing controlled substances via telemedicine, while individual states may impose additional restrictions on remote prescribing practices.
Controlled substance prescribing through telemedicine generally requires an established patient-provider relationship or specific emergency circumstances. The Ryan Haight Act mandates in-person evaluations before prescribing controlled substances in most telemedicine situations, though emergency exceptions and established patient relationships may provide limited flexibility.
Verify current DEA registration status covers telemedicine prescribing in all states where you treat patients. Maintain detailed documentation supporting the medical necessity for any controlled substance prescriptions issued through telemedicine encounters. Establish clear protocols for patient identity verification before prescribing any medications remotely.
Review state-specific prescribing regulations that may be more restrictive than federal requirements. Some states prohibit certain medication classes from being prescribed through telemedicine or require additional patient monitoring procedures. Create systematic processes for monitoring patient compliance with prescribed medications when follow-up occurs virtually rather than in person.
Implement secure prescription transmission methods that meet both state and federal requirements. Electronic prescribing systems must include appropriate authentication and audit trail capabilities. Patient counseling about prescribed medications should include specific instructions for safe storage and disposal, particularly important when patients receive medications without in-person pharmacy consultation.
State prescription monitoring programs may have specific reporting requirements for medications prescribed through telemedicine. Providers must ensure their prescribing practices comply with monitoring program requirements and maintain appropriate access to patient prescription histories.
Successful telemedicine implementation requires comprehensive legal preparation that addresses licensing, compliance, technology, and liability concerns before launching virtual care services. Many providers rush into telemedicine without adequate legal framework, creating unnecessary risks that could devastate their practice.
Professional liability insurance coverage must specifically include telemedicine services, as some policies exclude virtual care or provide limited coverage for remote patient encounters. Standard malpractice policies may not adequately protect providers from telemedicine-specific risks, requiring policy modifications or additional coverage.
Legal GPS offers specialized contract templates designed specifically for telemedicine practices, including comprehensive informed consent forms, patient privacy agreements, and vendor contracts that properly allocate technology-related liability. These templates address the unique legal requirements of virtual care that generic healthcare contracts often miss.
The regulatory landscape for telemedicine continues evolving rapidly, with new federal guidelines and state-specific requirements emerging regularly. Staying current with these changes requires ongoing legal education and systematic compliance monitoring that many busy providers struggle to maintain independently.
Your telemedicine legal foundation determines whether virtual care expands your practice successfully or exposes you to devastating liability. Investing in proper legal preparation protects your practice, your patients, and your professional future in an increasingly digital healthcare environment.
Don't let telemedicine legal risks undermine your practice success. Legal GPS Pro membership provides access to comprehensive telemedicine contract templates, regular regulatory updates, and expert guidance for navigating complex virtual care compliance requirements. Protect your practice with the legal framework you need to deliver telemedicine services safely and successfully.
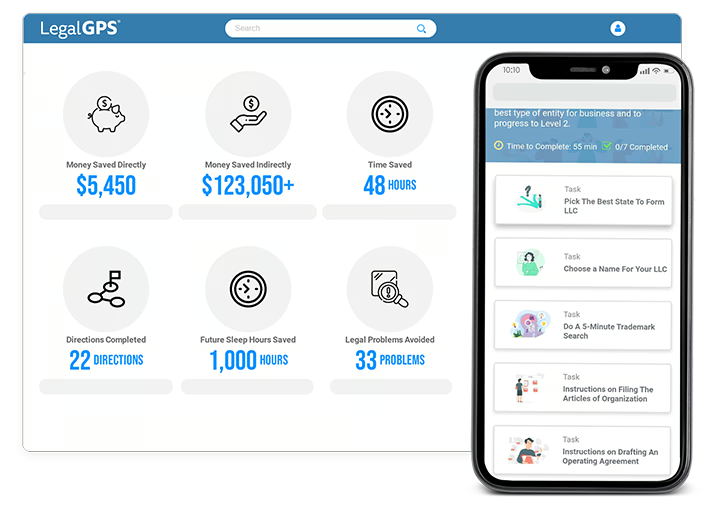
Legal GPS Pro
Protect your business with our complete legal subscription service, designed by top startup attorneys.
|
Premium Template
Single-use Template |
Legal GPS Pro
Unlimited Access, Best Value |
|
|
| Choose Template | Learn More |
| Trusted by 1000+ businesses | |
Table of Contents

Healthcare businesses face an increasingly complex regulatory landscape where a single compliance mistake can result in devastating financial...