Fitness Industry Lawsuits: What Personal Trainers and Clients Must Know
The fitness industry faces an unprecedented surge in legal challenges, with lawsuits against personal trainers, gyms, and fitness facilities...
9 min read
LegalGPS : Oct. 29, 2025
Mental health practitioners face unique liability risks that can devastate both their practice and personal finances. Unlike other healthcare providers, therapists navigate complex emotional boundaries, crisis interventions, and sensitive ethical obligations that create multiple exposure points for legal claims.

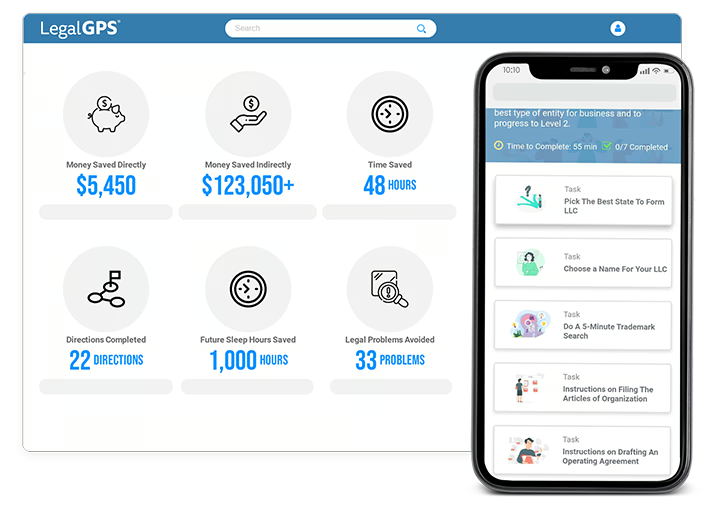
Legal GPS Pro
Protect your business with our complete legal subscription service, designed by top startup attorneys.
The financial stakes are substantial. Professional liability settlements in mental health cases average $175,000, with some reaching into the millions. More concerning is that standard malpractice insurance often contains gaps that leave practitioners personally liable for certain types of claims.
This comprehensive guide will walk you through proven strategies to minimize your liability exposure while maintaining the therapeutic relationships that make your practice successful. You'll learn specific documentation techniques, insurance requirements, and practice management protocols that have protected thousands of mental health professionals from costly litigation.
Mental health practitioners face liability exposure across multiple areas that traditional medical malpractice doesn't fully address. Understanding these risks is the first step toward building comprehensive protection.
The most common liability claims against mental health professionals include failure to prevent suicide, sexual misconduct allegations, breach of confidentiality, and improper treatment leading to patient deterioration. Unlike physical medicine where outcomes are often measurable, mental health treatment involves subjective assessments and long-term relationship dynamics that complicate liability determinations.
Professional licensing boards also create additional exposure through disciplinary actions that can impact your practice even when criminal charges aren't filed. These administrative proceedings follow different rules than civil courts and can result in license suspension or revocation based on preponderance of evidence rather than beyond reasonable doubt standards.
Dr. Sarah Martinez learned about liability exposure the hard way when a former patient filed a malpractice claim three years after treatment ended. The patient alleged that Dr. Martinez failed to properly assess suicide risk during their final session, leading to a suicide attempt two months later.
Dr. Martinez's clinical notes for that session contained only basic information: "Patient reports improved mood, scheduled for follow-up in two weeks." There was no documentation of specific suicide risk assessment questions, the patient's responses, or the clinical reasoning behind the treatment plan.
The plaintiff's attorney argued that this sparse documentation proved inadequate care. Without detailed notes showing proper risk assessment protocols, Dr. Martinez's insurance company settled the case for $340,000 rather than risk a larger jury verdict. The settlement also triggered a licensing board investigation that required additional legal fees and nearly resulted in practice restrictions.
Beyond direct treatment issues, mental health practices face liability exposure through business operations and staff management. Employment law violations, HIPAA breaches, and inadequate supervision of unlicensed staff create additional risk categories that many practitioners overlook.
Technology-related risks continue expanding as telehealth becomes more prevalent. Unsecured communication platforms, inadequate data encryption, and insufficient informed consent for remote services have generated new categories of liability claims. Even well-intentioned practitioners can face significant exposure when their technology practices don't meet evolving legal standards.
Mental Health Services Agreement defining scope, confidentiality, and provider responsibilities.
Trusted by 1,000+ businesses to safeguard their LLCs.
Standard professional liability insurance for mental health practitioners often contains significant gaps that can leave you personally responsible for certain types of claims. Understanding what your policy covers and doesn't cover is crucial for adequate protection.
Your policy should include coverage for professional services, administrative errors, and cyber liability incidents. The minimum coverage amount should be $1 million per incident with $3 million aggregate annually, though higher limits are advisable for group practices or those working with high-risk populations.
Defense cost coverage structure significantly impacts your financial exposure. "Defense costs within limits" policies reduce your available settlement funds as legal fees accumulate, while "defense costs in addition to limits" policies provide separate funding for attorney fees. The premium difference is usually modest compared to the protection difference.
Most standard policies exclude claims related to sexual misconduct, criminal acts, and business disputes with partners or employees. You need separate employment practices liability insurance and potentially additional coverage for false allegations of inappropriate conduct.
Licensing board defense coverage is often optional but essential. Administrative proceedings can cost $50,000 or more in legal fees even when no wrongdoing occurred. This coverage pays for attorneys experienced in licensing law rather than forcing you to use your general practice lawyer.
Retroactive date coverage protects you from claims arising from services provided before your current policy began. When changing insurers, ensure your new policy covers all your prior professional activities or maintain extended reporting coverage from your previous carrier.
Dr. Michael Chen discovered his coverage gaps when a former employee filed a wrongful termination lawsuit combined with allegations of inadequate clinical supervision. The employee claimed that Dr. Chen's oversight failures contributed to a patient safety incident.
Dr. Chen's professional liability policy covered the clinical supervision allegations but excluded the employment law claims. His business insurance covered employment disputes but excluded professional liability issues. The overlapping nature of the claims meant both insurers denied coverage for portions of the case.
Dr. Chen ultimately paid $85,000 in legal fees and settlements from personal funds. He now carries employment practices liability insurance and ensures his professional liability policy includes supervisory liability coverage for all staff members.
Thorough documentation serves as your primary defense against liability claims while supporting quality patient care. Your records should tell a complete story of your clinical decision-making process and demonstrate adherence to professional standards.
Every patient encounter should include assessment findings, treatment interventions, patient responses, and plans for future care. Risk assessment documentation requires particular attention, especially for suicide risk, violence potential, and substance abuse issues. Your notes should reflect specific questions asked, patient responses, and the clinical reasoning behind your risk level determination.
Progress notes must be contemporaneous, meaning written within 24 hours of the patient encounter. Delayed documentation raises questions about accuracy and completeness that can undermine your credibility in litigation. Electronic health record timestamps can prove when notes were actually created, making timely documentation even more critical.
When a patient's family sued Dr. Lisa Rodriguez after their daughter's suicide, her detailed documentation proved crucial to her defense. Her notes showed consistent suicide risk assessments using standardized screening tools, documented safety planning discussions, and clear reasoning for treatment modifications.
Specific documentation included the patient's exact responses to suicide screening questions, family members' observations during sessions, and collaboration notes with the prescribing psychiatrist. Dr. Rodriguez also documented her consultation with a colleague about the case and the continued assessment that led to her treatment recommendations.
The thorough documentation demonstrated that Dr. Rodriguez had followed established protocols and made reasonable clinical decisions based on available information. The plaintiff's experts couldn't identify any documentation failures or treatment standard deviations. The case was dismissed on summary judgment without requiring a trial.
Electronic health records create new documentation challenges and liability exposures that weren't issues with paper charts. Your record system must include audit trails showing who accessed what information and when, automatic backup procedures, and secure transmission capabilities for sharing information with other providers.
HIPAA compliance extends beyond just securing patient information to include staff training, business associate agreements, and breach notification procedures. Even minor violations can trigger federal investigations and substantial penalties that professional liability insurance typically doesn't cover.
Cloud-based storage and telehealth platforms require particular attention to data security requirements. Your business associate agreements must specify security standards and breach notification procedures. Many practitioners assume their technology vendors handle all compliance issues, but ultimate responsibility remains with your practice.
Implement a practice standard requiring all clinical documentation within 24 hours of patient contact. This includes therapy sessions, phone consultations, and crisis interventions. Use electronic calendar reminders or other systems to ensure compliance rather than relying on memory.
When documentation delays are unavoidable due to emergencies or technical issues, create an addendum explaining the delay and confirming that the notes reflect your contemporaneous recollection of the encounter. Never backdate documentation or alter existing records without clear addendum procedures that maintain record integrity.
Clear boundaries and comprehensive informed consent procedures prevent many liability issues while supporting therapeutic relationships. Your informed consent process should address treatment methods, confidentiality limits, emergency procedures, and fee arrangements in language patients can understand.
Treatment agreements should specify your availability between sessions, emergency contact procedures, and policies for missed appointments or treatment non-compliance. These agreements protect both you and your patients by establishing clear expectations and reducing potential misunderstandings.
Dual relationships require careful navigation even when not explicitly prohibited by your licensing board. Social media connections, business relationships, and community interactions can create ethical complications that lead to licensing complaints or civil liability. Establish clear policies about boundary management and document any boundary crossings with their clinical justification.
Dr. Amanda Foster faced a malpractice claim when her treatment relationship with a patient became complicated by social connections. She treated the patient's daughter while also serving on a nonprofit board with the patient. The overlapping relationships created conflicts when the treatment wasn't progressing as expected.
The patient alleged that Dr. Foster's board relationship compromised her clinical judgment and led to inappropriate treatment recommendations. Although Dr. Foster had documented her awareness of the dual relationship and consultation with colleagues about managing it, the complexity of the situation contributed to treatment difficulties.
The case ultimately settled for $125,000 because the dual relationship created questions about Dr. Foster's objectivity and professional boundaries. Her insurance company determined that defending the case would cost more than settlement, even though no clear standard of care violations occurred.
When dual relationships are unavoidable in small communities, document your assessment of potential conflicts and consultation with colleagues about managing the situation. Consider whether referral to another provider would better serve the patient's interests, even if it creates personal or financial inconvenience.
Referral procedures should include clear criteria for when referrals are necessary, how to handle patient resistance to referral, and documentation requirements for referral decisions. Your malpractice exposure can continue even after referral if you don't properly transfer care or continue to provide advice to the patient.
Crisis situations create the highest liability exposure for mental health practitioners while demanding immediate responses that don't allow time for careful legal consultation. Established protocols help you respond appropriately while protecting yourself from second-guessing during litigation.
Suicide risk assessment requires standardized protocols that go beyond clinical intuition. Use validated screening instruments like the Columbia Suicide Severity Rating Scale and document specific risk factors, protective factors, and safety planning measures. Your assessment should address immediate risk, ongoing monitoring needs, and family involvement in safety planning.
Dr. James Park's crisis response protocols proved essential when a patient called threatening suicide on a Friday evening. Dr. Park's established procedures included specific questions to assess imminent risk, clear criteria for emergency interventions, and documented decision trees for different risk levels.
Following his protocol, Dr. Park assessed the patient's access to lethal means, substance use, and social support availability. The patient had a specific plan but agreed to safety measures including removing firearms from his home and staying with family members over the weekend. Dr. Park documented the entire conversation and his clinical reasoning for not initiating involuntary commitment.
When the patient later sued claiming inadequate emergency response, Dr. Park's detailed crisis documentation and evidence-based protocols demonstrated appropriate care. Expert witnesses testified that his response met professional standards and likely prevented a suicide attempt. The case was dismissed without settlement.
Child abuse reporting requirements create potential liability from both failure to report suspected abuse and improper reports that aren't supported by evidence. Understand your state's specific reporting requirements, including timeframes for reports and documentation standards for suspected abuse.
Elder abuse and domestic violence reporting requirements vary significantly by state and practitioner license type. Some states require reports only when patients are in immediate danger, while others mandate reporting whenever abuse is suspected. Consult with legal counsel about your specific obligations rather than assuming requirements are uniform.
Create a standardized crisis documentation template that includes risk assessment questions, safety planning elements, and follow-up procedures. Use this template consistently for all crisis interventions to ensure comprehensive documentation and defensible decision-making.
Your crisis documentation should include verbatim quotes when possible, especially regarding statements about self-harm or violence toward others. Document who else you consulted during the crisis, what resources you recommended, and specific follow-up plans including timing and responsibility assignments.
Your business entity structure affects your personal liability exposure for practice-related claims. Professional corporations and limited liability companies can provide asset protection while maintaining professional licensing requirements, but the protection varies significantly by state law.
Professional liability insurance protects you from malpractice claims but doesn't cover business disputes, employment law violations, or general liability issues. Your practice needs multiple insurance layers including general liability, employment practices liability, and cyber liability coverage to address different risk categories.
Employment practices become more complex as your practice grows to include multiple therapists, administrative staff, and supervisees. Clear policies about supervision requirements, scope of practice limitations, and documentation standards help prevent claims while ensuring quality patient care.
Dr. Patricia Wells' professional corporation structure protected her personal assets when her practice faced a complex malpractice claim involving multiple therapists and supervisory issues. The claim alleged inadequate supervision of an unlicensed therapist who provided inappropriate treatment to a trauma patient.
The corporate structure meant that Dr. Wells' personal assets including her home and retirement accounts were protected from the business liability. Her professional liability insurance covered the clinical aspects of the claim, while the corporate structure contained the financial exposure to practice assets.
Without the corporate protection, Dr. Wells could have faced personal liability exceeding $2 million for the supervisory failures and business operations issues. The case ultimately settled within insurance limits, and Dr. Wells continued practicing without personal financial impact.
The key to liability protection is implementing comprehensive risk management before problems arise. This includes appropriate insurance coverage, sound documentation practices, clear policies and procedures, and regular consultation with legal and insurance professionals who understand mental health practice issues.
Legal GPS offers specialized templates and resources designed specifically for mental health practitioners, including informed consent forms, crisis protocols, and business structure guidance. Our Pro subscription provides ongoing updates as laws change and new liability issues emerge in mental health practice.
Remember that liability protection is an ongoing process, not a one-time setup. Regular reviews of your insurance coverage, documentation practices, and practice procedures help ensure continued protection as your practice evolves and legal requirements change.
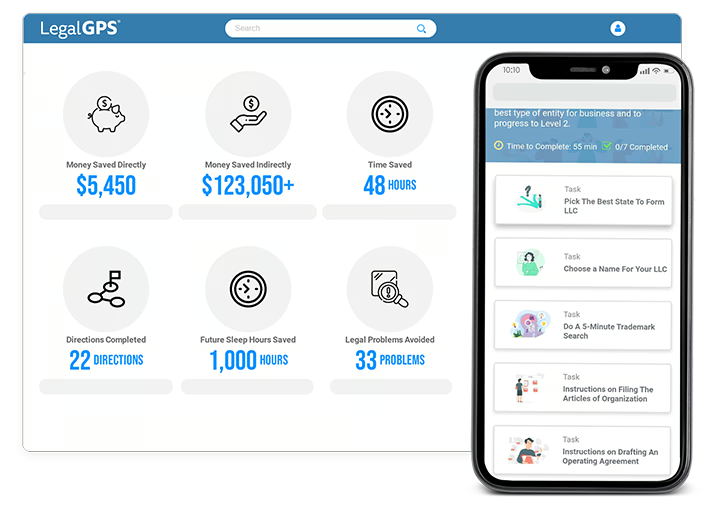
Legal GPS Pro
Protect your business with our complete legal subscription service, designed by top startup attorneys.
|
Premium Template
Single-use Template |
Legal GPS Pro
Unlimited Access, Best Value |
|
|
| Choose Template | Learn More |
| Trusted by 1000+ businesses | |
Table of Contents

The fitness industry faces an unprecedented surge in legal challenges, with lawsuits against personal trainers, gyms, and fitness facilities...

Running a business while caring for a beloved pet creates unique challenges that many entrepreneurs face daily. The solution often involves hiring...

The pet care industry has exploded into a $261 billion global market, with millions of families trusting strangers with their beloved animals every...